- Home
- Elbow Pain Diagnosis
- Wrist Fractures
Distal Radius Fracture
Written By: Chloe Wilson BSc (Hons) Physiotherapy
Reviewed By: SPE Medical Review Board
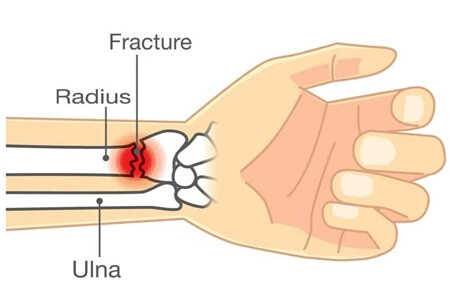
A distal radius fracture, aka wrist fracture, is a common injury to one of the forearm bones, near the wrist.
Distal radial fractures typically occur when there is a fall onto an outstretched hand, but they can also result from direct trauma to the wrist e.g. sports or road traffic accidents.
Wrist fractures are very common accounting for around 15-20% of all fractures treated in emergency departments. In fact, the distal radius is the most common bone to break in the arm.
There are lots of different types of distal radial fracture including Colles fracture and Smiths fracture.
Here we will look at the common causes, symptoms and diagnosis for the different types of distal radius fracture and best treatment options for each.
Wrist Fracture Anatomy
Quick anatomy lesson to set the scene. There are two long bones in the forearm that run between the elbow and the hand:
- Radius: is located on the thumb side (lateral aspect). It widens out at the wrist forming a large bony prominence, the radial styloid process, on the outer side of the wrist which forms the bulk of the wrist joint aka radiocarpal joint
- Ulna: is located on the pinky side (medial aspect). It is much narrower than the radius at the wrist and has a small bony prominence, the ulna styloid, on the inner side of the wrist
The distal part of the radius refers to the end nearest to your wrist. The radius is responsible for forearm rotation (turning your palm up and down) and supports the majority of the forces through the wrist joint.
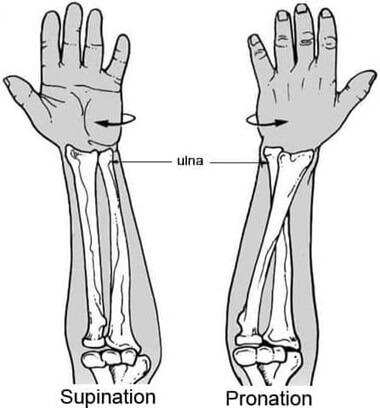
The radius and ulna run parallel to each other when in a neutral position (supination) i.e. palm facing up, but when you twist your wrist so the palm faces down (pronation), the radius rotates to cross over the top of the ulna.
Both the radius and ulna are essential for the function and stability of the forearm and wrist.
Their coordinated movements enable actions such as flexion, extension, pronation, and supination of the forearm, contributing to the versatility and dexterity of the upper limb.
What Is A Distal Radius Fracture?
A distal radius fracture refers to a break towards the end of the radius bone, near the wrist.
Most distal radial fractures occur about 1 inch above the wrist joint. Typically there is a complete break in the radius, i.e. it breaks into two or more pieces, although smaller hairline fractures can occur, usually from repetitive overuse.
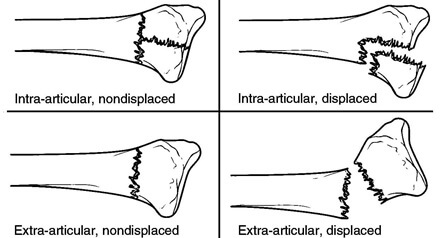
Distal radius fractures can be characterised as:
- Displaced or Non-Displaced: with a non-displaced fracture of distal radius, the bone fragments remain in alignment - there is no significant shifting or separation of the fractured ends. With a displaced distal radius fractures involve a significant separation or displacement of the broken bone fragments so they are out of alignment
- Closed Or Open Fracture: A closed fracture distal radius, aka simple fracture, is when the bone is broken, but the skin is intact. An open distal radius fracture, aka compound fracture, is when the broken bone pokes through the skin. An open fracture requires immediate medical attention as there is a high risk of infection
- Intra-Articular or Extra-Articular: An intra-articular distal radius fracture is where the break extends into the wrist joint, affecting the articular surface. It tends to take a high-energy trauma to cause an intra-articular distal radial fracture so is more common in younger people. A distal radius extra-articular fracture is where the break occurs outside the wrist joint, so the articular surface is unaffected. Most distal radius fractures are extra-articular
- Comminuted Fracture: if the distal radius is broken in more than two places, resulting in multiple bone fragments, it is referred to as a comminuted distal radius fracture
Classifying distal radius fractures is important as the different types of fractures will be treated differently. Displaced, open, intra-articular and comminuted fractures are generally more difficult to treat than non-displaced, closed, extra-articular distal radius fractures.
Types Of Distal Radius Fracture
There are four main types of distal radial fracture:
- Colles Fracture: The most common type of distal radius fracture is a Colles fracture. Colles fractures happen when the wrist is forcibly extended e.g. fall onto an outstretched hand. With a Colles fracture, the distal end of the radius breaks and the fracture fragment is displaced dorsally (towards the back of the hand), tilting upwards, often resulting in a characteristic “dinner fork” deformity at the wrist. They are extra-articular.
- Smith’s Fracture: aka reverse Colles fracture, a Smith’s fracture occurs when the wrist is forcibly flexed. The distal end of the radius breaks and the fracture fragment displaces volarly (towards the palm). Smith’s fractures are much less common than Colles fractures but can also result in significant wrist deformity. Extra-articular.
- Barton’s Fracture: a fracture of the distal radius with associated dislocation of the radiocarpal joint, the joint between the radius and 1st row of the hand bones. Intra-articular
- Hutchinson Fracture: aka Chauffeur’s fracture, this type of distal radius fracture involves a break of the radial styloid process, the bony prominence on the outer side of the wrist. Intra-articular.
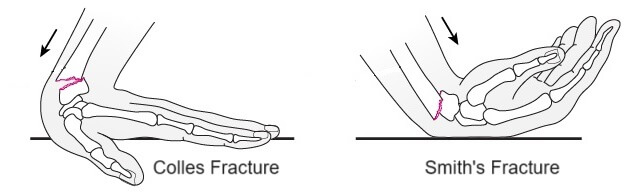
The most common type of distal radius fracture is a Colles Fracture, accounting for 90% of wrist fractures.
Common Causes Of Distal Radius Fracture
A distal radius fracture is usually caused by:
- A Fall: The most common cause of a distal radius fracture is a fall onto an outstretched hand, where the wrist is forced backwards. This typically results in a Colles fracture. A fall onto a flexed hand, where the wrist is forced forwards usually results in a Smith’s fracture. If you fall, your natural instinct is to try and break your fall by thrusting your hands out to catch you, which puts significant force through the wrist joint, often resulting in a distal radial fracture
- Sports Injuries: Distal radius fractures are common in high impact or contact sports such as football, basketball, skiing, cycling and skateboarding due to falls, collisions or a forceful blow to the wrist
- Motor Vehicle Accidents: Injuries sustained during motor vehicle accidents, particularly when the hands are braced against the steering wheel or dashboard upon impact, can cause distal radius fractures
- Osteoporosis: a bone disorder commonly associated with aging, where changes in bone structure and density result in weakened, more brittle bones. People with osteoporosis have a higher risk of distal radius fractures, especially in situations where minimal force is applied e.g. minor falls from a standing height, as it takes less force for the bones to break
- Aging: Older adults are more prone to distal radius fractures due to age-related changes in bone density and strength, even if they don’t have osteoporosis. As people age, their bones become more brittle and less able to withstand impact, increasing the risk of fractures, even from relatively minor falls or trauma. Distal radial fractures in young adults usually only occur with high-energy trauma e.g. when falling from a height such as out of a tree, whereas elderly people may sustained a distal radial fracture from a relatively minor fall e.g. tripping over from standing height
- Repetitive Stress: Certain repetitive activities or motions that put stress on the wrist joint over time can increase the risk of developing stress fractures or micro-fractures in the distal radius. This is more common in athletes or individuals who engage in repetitive tasks that involve the wrist, such using hand tools
Common Symptoms
Common symptoms of a distal radial fracture include:
- Pain: The most prominent symptom of a distal radius fracture is pain at the site of the injury. There is usually immediate pain at the time of injury and there is often tenderness over the area when touched
- Swelling: With distal radial fractures, there is often significant swelling in the wrist that may extend up the forearm or into the hand. The swelling usually occurs immediately at the time of injury, or certainly within a few hours
- Bruising: Bruising or discoloration of the skin around the wrist and forearm may develop due to bleeding from the fractured bone or surrounding soft tissues
- Deformity: Often with wrist fractures, particularly with displaced fractures, there may be a visible deformity or misalignment of the wrist. This can manifest as an abnormal angle or shape of the wrist. With a Colles fracture there is often a distinct bump in the wrist resembling the neck of a fork, commonly referred to as a “dinner fork” deformity, whereas with a Smith fracture there is usually a distinct drop in the wrist
- Restricted Range Of Motion: A distal radial fracture can restrict movement of the wrist and forearm, leading to difficulty bending, straightening, or rotating the wrist. Severe pain or instability may further limit range of motion
- Numbness Or Tingling: With more severe distal radius fractures, there may be some compression or injury to nearby nerves which can lead to sensations of numbness, tingling or weakness in the hand and fingers
It is important to note that not all distal radius fractures present with the same symptoms, and the severity and combination of symptoms experienced may vary. Age, medical conditions, and the cause of injury can affect symptoms.
Seek immediate medical attention if you suspect a distal radius fracture or experience any of these symptoms after a wrist injury to ensure proper diagnosis and treatment.
Diagnosis
Early diagnosis and treatment is really important with a distal radius fracture. Your doctor will start by taking a history to find out about the mechanism of injury, relevant medical conditions, previous injuries etc.

They will then examine your wrist looking for any swelling, bruising, tenderness, movement restriction, altered sensation and weakness as well as any obvious deformities like the classic dinner fork deformity.
If your doctor suspects a distal radius fracture they will send you for imaging studies, usually an x-ray which will show any breaks in the bone, loose fragments and the degree of displacement. For more complex injuries, you may also be sent for an MRI or CT scan for more detailed images.
Distal Radius Fracture Treatment
The best treatment for a distal radius fracture will depend on:
- Bone Displacement: how much the bones have shifted
- Comminution: the degree of fragmentation i.e. how may breaks there
- Joint Involvement: if there is damage to the articular surface of the wrist joint
- Associated Injuries: soft tissue damage, nerve damage, damage to circulatory system, other fractures etc.
- Individual: age, activity level, hand dominance, general health, functional goals etc.
The primary goal with a wrist fracture is to correct any displacement by putting the bones back into the right place and then holding them there, either with a splint, cast or surgical stabilisation while they heal.
Non-Surgical Treatment
Non-surgical treatment for a distal radius fracture usually involves:
- Closed Reduction: If there is some displacement of the radius, the doctor will re-align the bone fragments through traction and manipulation, by pulling or pushing on the ends of the fractured bone until they line up correctly. Typically you will be awake during the procedure but you will be given medication to help you relax and to control the pain e.g. local anaesthetic. They will re-xray your wrist to ensure the bones are in the correct position.
- Splint/Cast: If there is no displacement, or once the bones have been realigned with a closed reduction, then a cast or splint will be applied to hold the bones in the correct position while the fracture heals. The cast may stop just below your elbow or may extend above the elbow to provide additional stability. You may start with a temporary, removable cast (aka backslab) or splint for the first week or so while the swelling goes down, at which point a fixed cast is usually fitted for 4-6 weeks. Further x-rays will be taken to check the fracture has healed before removing the cast. You may then be given a removable splint to wear for a few weeks to support the wrist. It is really important to keep your cast dry so take care when washing. You can get special cast covers that keep your cast dry when washing which can be really helpful.
Surgical Treatment
Some types of wrist fracture, e.g. complex comminuted or intra-articular distal radius fractures, cannot be correct without the need for surgery. If the bones can’t be realigned properly or held in place sufficiently well with a cast, then there is a high risk of the fracture healing in a poor position which can lead to ongoing problems with hand function. Surgery is therefore recommended.
Distal radius fracture surgery should be carried out as soon as possible, certainly within 2 weeks of injury, before early bone healing begins. There are a few different surgical options with distal radial fractures:
1. Open Reduction Internal Fixation (ORIF)
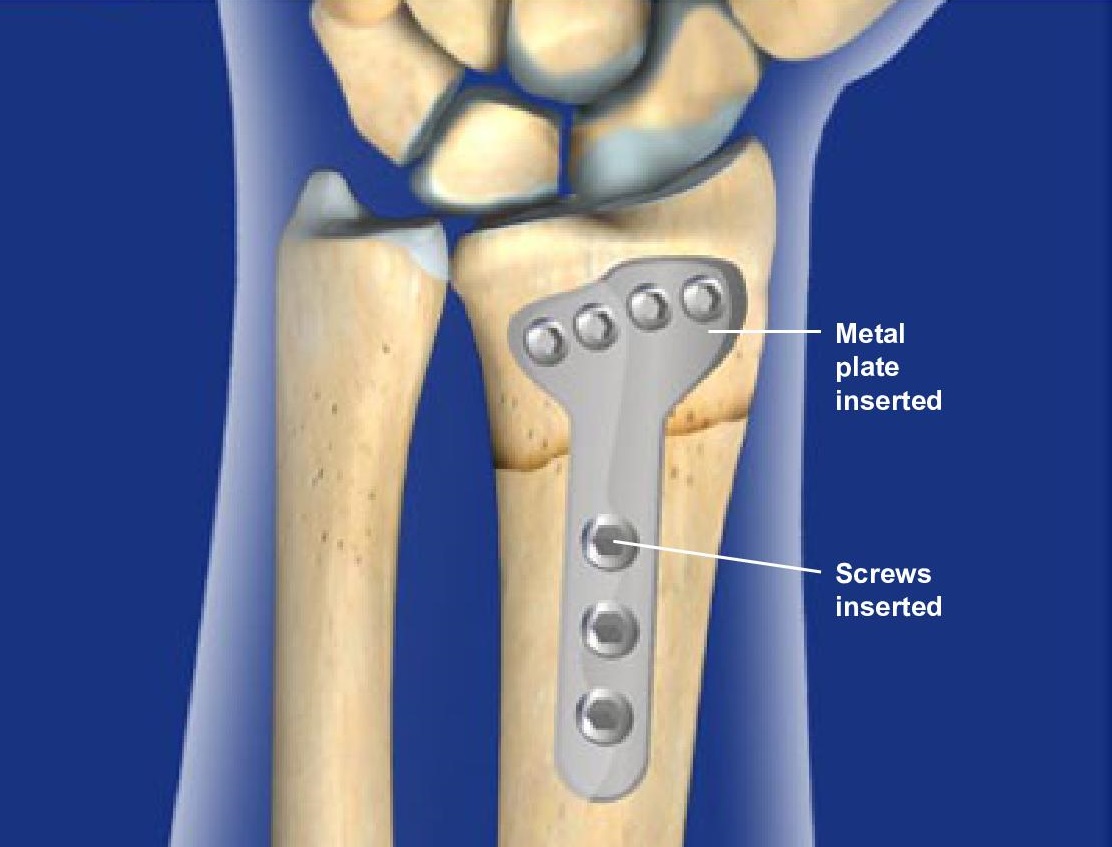
With open reduction internal fixation (ORIF) surgery for a distal radius fracture, an incision is made over the fracture site, usually on the front of the wrist (palm side).
This allows the surgeon to directly visualize and manipulate the fracture fragments back into proper alignment.
Once the fragments are aligned, specialized hardware e.g. plates, screws or pins are used to hold the fragments in place while the fracture heals. The wrist will be immobilised in a cast or splint usually for around 3 weeks.
In most cases, the hardware is left in place even once the wrist fracture has healed, unless it starts causing problems.
2. External Fixation
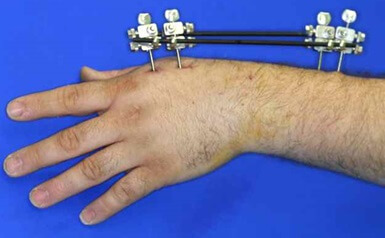
With external fixation surgery for distal radius fractures, the bones are typically realigned with closed reduction.
Pins or wires are then inserted into the bone each side of the fracture site and then connected to a rigid external frame that holds everything stable.
The surgeon may use bridging external fixation which extends across the wrist joint, or non-bridging external fixation which does not cross the wrist. Kirschner wires, aka k-wires may also be used along with the external fixator for extra stability. Once the fracture has healed, the metalwork is removed.
3. Percutaneous Pinning

With percutaneous pinning of a distal radius fracture, a closed reduction of the fracture is performed and then percutaneous pins (thin wires) are inserted through the skin and into the bone to maintain alignment.
The wrist is then placed in a cast for 3-6 weeks. This is less invasive than open fixation as no incision is required, the pins are simply pushed through the skin into place - they may be completely buried or may extend out of the skin.
Whichever type of surgical treatment is used for a distal radius fracture, the cast or external fixator will be removed once there is confirmation by x-ray that the fracture has healed. This usually takes between 3 and 6 weeks depending on the fixation method.
Distal Radius Fracture Recovery Time
Distal radius fracture recovery time will depend on the severity of the break, the treatment method used and the age and health of the individual.
The goals of treatment are to realign the bones and regain full movement and function in the wrist and hand. Whether surgery is necessary or not, there are lots of things you can do to help improve distal radius fracture recovery time:
#CommissionsEarned from Amazon on qualifying purchases
1. Swelling Management
It is really important to reduce the amount of swelling with a distal radial fracture to reduce pain, speed up healing and promote recovery of normal hand function.
You can help to drain excess fluid away by keeping the hand raised above the level of your heart whenever possible and keep the fingers and thumb moving regularly. If you notice your fingers are swelling, you can massage them with long firm strokes from your fingertips, down towards you wrist.
2. Hand & Arm Movements
Whilst wearing the cast, it is really important to keep your fingers, thumb, elbow and shoulder moving normally as much as you are able to. Not only does the help prevent stiffness and weakness, it also helps to reduce swelling.
People are often worried about using their affected arm after a distal radius fracture but the cast will hold your wrist bones completely still, so you don’t need to worry about damaging your wrist.
Simple exercises such as making a fist, touching your thumb to tips and bases of each finger, bending and straightening the elbow and moving and circling the shoulder can really help.
3. Physical Therapy
Once the cast has been removed, you will work with a physical therapist on a rehab program to restore full strength, stability and function in your forearm, wrist and hand. This usually involves a combination of strengthening, stretching, gripping and functional exercises.
There is a really useful booklet and videos from the NHS University Hospitals Sussex, UK that goes through what exercises to do at what stages with a distal radius fracture that we would highly recommend
4. Scar Massage

If you have undergone surgery, once the cast or external fixator is removed, it is helpful to regularly massage the scar to promote healing, reduce swelling and improve flexibility.
Using firm pressure, apply deep circular massage to the scar and surrounding are for 3-5 minutes, two or three times a day. This helps to keep the tissue around the scar loose and flexible. It often helps to use a light moisturiser when massaging the scar to reduce friction.
In some cases, the area around the scar is hyper-sensitive when the cast is first removed, in which case, gently stroking the affected area, or rubbing materials of different textures over the scar helps the area to adapt to normal stimulus and reduce sensitivity.
5. Pain Relief
It is normal to have some ongoing pain following a distal radial fracture than may persist for a number of months. Don’t worry, this is normal. Over the counter medications such as paracetamol and ibuprofen can help, as can regular ice packs in the early stages, and heat packs in the later stages.
6. Returning To Activities
In most cases, as soon as your cast/fixation device are removed, you can start using your injured wrist in normal light daily activities such as washing and dressing, dusting, using a keyboard and washing up and drying up. The more you use your wrist, the faster your distal radius fracture recovery time will be.
You may be given a removable splint to wear initially but it is important to try and wean yourself off this quickly. Start by taking it off when you are at home and then aim to stop wearing it when you are out and about. You can gradually increase the amount of weight you carry as comfortable and most people can return to sports around 12 weeks after injury.
7. Driving
In terms of driving, you should contact your insurance provider as your injury may affect your insurance. Most people can return to driving around 6-8 weeks post-injury. You need enough strength and flexibility in your wrist and hand to fully turn the wheel and change gear, and should make sure you can perform an emergency stop before driving.
8. Healing Time
When thinking about what is going on in the bone in terms of distal radius fracture recovery time, it usually takes 4-6 weeks for the bone to knit back together during which time it is really important not to move the wrist – that is why you are put in a splint, cast or external fixator. During this phase, the body is laying down new bone to bridge the gap, so the wrist needs to be kept still so as not to dislodge the healing bone.
However, once the bone has knit back together, this new bone bridge needs to strengthen. The bone gets stronger by being used and it is important to put the right stresses and strains through the area to that everything heals properly. So don’t be afraid to use you hand and wrist. You are actually helping it but getting it moving again. Expect some stiffness and discomfort when the cast is first removed – that is completely normal and doesn’t mean there is anything wrong. But don’t be afraid to get going.
A good guide is, if it’s a bit uncomfortable when doing something, pain level up to around 5/10, but the pain settles within 30 minutes of stopping the activity, that is ok. If however, the pain persists for more than an hour or two that is your body telling you are overdoing it, so ease off. If you are regularly experiencing significant pain, or pain persists for a significant amount of time after exercise or light use, contact your doctor and get checked out.
Distal Radius Fracture Summary
A distal radius fracture is a break in the outer forearm bone near the wrist.
Distal radial fractures are the most common type of fracture seen in emergency rooms accounting for around 20% of all fractures.
The most common cause of a distal radius fracture is a fall. In younger people, it tends to be a high-energy impact e.g. a fall from a height or road traffic accident whereas in more elderly people a simple fall from standing height often results in a wrist fracture.
There are four different types of distal radius fracture depending on the location and direction of the break – the most common is a Colles Fracture
Common symptoms of a distal radial fracture include deformity (most typically a dinner fork deformity) bruising, swelling and pain.
Distal radius fracture treatment starts with reducing the fracture to realign the bones and then holding the bones in place, either with a cast or with metal wear.
Distal radius fracture recovery time involves a combination of physical therapy, exercises, medication, elevation and graded return to activities, all of which aim to restore full range of motion, strength and stability in the wrist and hand.
You may also be interested in the following articles:
Page Last Updated: March 21st, 2024
Next Review Due: March 21st, 2026
Medical & Scientific References
- Distal Radius Fractures. University Hospitals Sussex NHS Foundation Trust
- Fractures Of Distal Radius: An Overview. Journal of Family Medicine & Primary Care
- External fixation versus volar locking plate for displaced intra-articular distal radius fractures: a prospective randomized comparative study of the functional outcomes. Journal Of Orthopedics & Traumatology
- External Fixation Techniques for Distal Radius Fractures. Clinical Orthopaedics & Related Research