- Home
- Common Shoulder Problems
- Dislocated Shoulder
Dislocated Shoulder
Written By: Chloe Wilson BSc (Hons) Physiotherapy
Reviewed By: SPE Medical Review Board
A dislocated shoulder is a common and painful injury that many people, of all ages, experience each year. It happens when the upper arm bone pops out of its socket in the shoulder. Shoulder dislocations can cause severe pain and make it hard to do everyday activities.
The shoulder joint is the most mobile and flexible joint in the body, which means it can move in many directions, but it's also the least stable. This means it's more prone to dislocations, especially when the joint is put under significant force e.g. a fall, sports injury or accident.
Here we will look at the common causes, symptoms and diagnosis of a dislocated shoulder, including the different types of shoulder dislocation that can occur. We will then go on to look at the different treatment options and the recovery process.
What Is A Dislocated Shoulder?
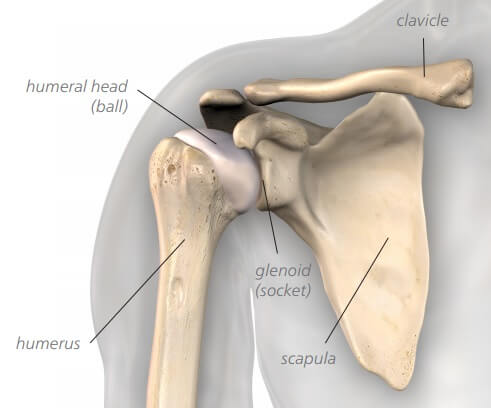
The shoulder joint, also known as the glenohumeral joint, is located between the upper arm bone (humerus) and the shoulder blade (scapula).
At the top of the upper arm bone is a rounded, ball-like structure called the humeral head. This ball-shaped part of the humerus fits into a socket on the shoulder blade known as the glenoid.
A dislocated shoulder is where the humeral head is forced out of its normal position in the glenoid socket. There shoulder joint may dislocated partially or fully:
- Partial Shoulder Dislocation: aka subluxation, occurs when the humeral head partially dislodges from the joint but does not completely come out of the socket. It usually returns to the socket on its own or with minimal assistance
- Complete Shoulder Dislocation: when the humeral head comes completely out of the joint, so the ball and socket are no longer in contact at all. A full shoulder dislocation needs immediate medical attention and will not relocate on its own
The shoulder joint has a unique design that prioritizes mobility and flexibility. Unlike other ball and socket joints in the body e.g. the hip, the socket is extremely shallow which allows for the huge amount of movement at the shoulder. Just think about how much motion you have at your shoulder compared to your hip.
However, this immense range of motion comes at that sacrifice of stability. The body compensates for this with a complex system of ligaments, cartilage and muscles to hold the joint together but this lack of stability puts the shoulder at greater risk of dislocation.
Types Of Shoulder Dislocation
There are three different types of shoulder dislocation relating to the direction of displacement of the joint:
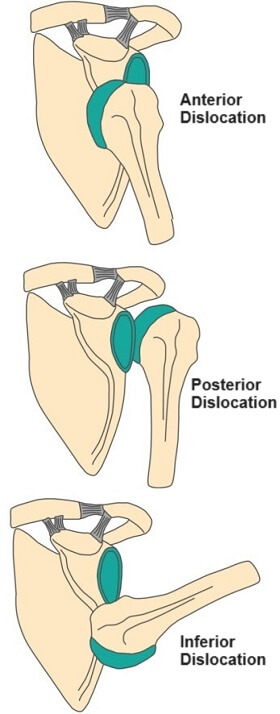
- Anterior Shoulder Dislocation: In an anterior shoulder dislocation the humeral head is forced forwards and away from the glenoid socket. This often results in a visible bump or deformity in the front of the shoulder, making it look like the shoulder has a hump or a bulge. The arm may also appear slightly outwardly rotated. This is the most common type of shoulder dislocation
- Posterior Shoulder Dislocation: In a posterior shoulder dislocation, the humeral head is forced backwards, towards the back of the shoulder blade. This type of dislocation is less common but can be more challenging to diagnose because the deformity may not be as obvious. The affected arm may appear internally rotated
- Inferior Shoulder Dislocation: An inferior shoulder dislocation is rare and involves the humeral head moving downwards. This type of dislocation can be particularly painful and may cause the arm to hang limply at the side. It can be challenging to distinguish inferior dislocations from other types of shoulder injuries
What Causes Shoulder Dislocation?
There are a number of possible shoulder dislocation causes including:
- Trauma: High-impact accidents and falls, are common causes of shoulder dislocation. A forceful impact or blow to the shoulder, such as a collision with an object or another person, can push the humerus out of its normal position in the glenoid socket. A fall onto an out-stretched arm or from a great height can generate enough force to dislocate the shoulder
- Sports Injuries: certain sports, particularly those involving physical contact or overhead arm movements e.g. football, rugby, wrestling, skiing and swimming increase the risk of shoulder dislocations
- Overhead Arm Movements: activities that involve sudden or forceful overhead arm movements, such as throwing a ball or reaching for an object on a high shelf, can cause shoulder dislocations. These movements can cause the humeral head to slip out of the socket, especially if combined with external rotation and abduction of the arm
- Repetitive Strain: Over time, repetitive overhead motions, e.g. baseball pitching or swimming, can weaken the stabilizing structures of the shoulder resulting in wear and tear. This leads to joint instability and makes the shoulder more susceptible to dislocations
- Muscle Imbalance: An imbalance in the strength and coordination of the muscles around the shoulder joint can lead to instability. Weakness, fatigue, overuse or improper conditioning of certain muscles can disrupt the dynamic support needed to keep the humeral head centered in the glenoid socket resulting in adequate support
- Congenital or Anatomical Factors: Some individuals have naturally looser or more hypermobile joints, shallower glenoid sockets, or other structural variations that predispose them to shoulder dislocations
- Previous Dislocations: If an individual has experienced a previous shoulder dislocation, they are at a higher risk of future dislocations. Repeated dislocations can damage the supportive structures of the shoulder, making it more unstable
- Violent Muscle Contractions: In rare cases, shoulder dislocations can occur due to non-traumatic events, such as seizures, severe muscle spasms or electric shocks. These events can lead to sudden and forceful muscle contractions that overpower the stabilizing muscles around the shoulder joint
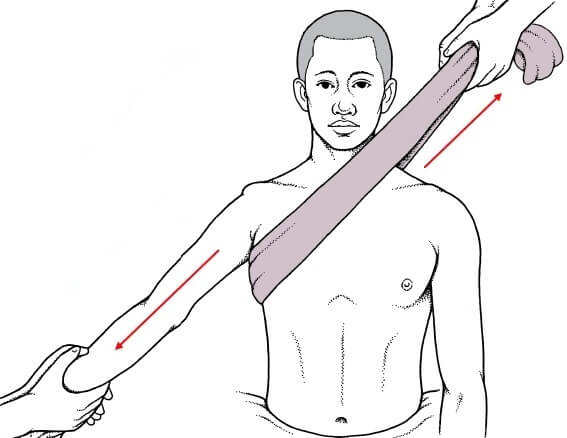
The most common mechanism for an anterior shoulder dislocation is a force that drives the humerus into external rotation and abduction. This often occurs when the arm is extended outward and experiences a sudden blow or impact to the front of the shoulder.
Posterior shoulder dislocations are less common but often result from a force that drives the humerus into internal rotation. This can happen during activities where the arm is forcefully pushed or twisted inwards.
Dislocated Shoulder Symptoms
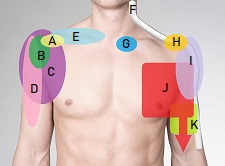
A dislocated shoulder can cause a range of symptoms, which can vary in intensity depending on the severity of the dislocation and whether any associated injuries have occurred. Common dislocated shoulder symptoms include:
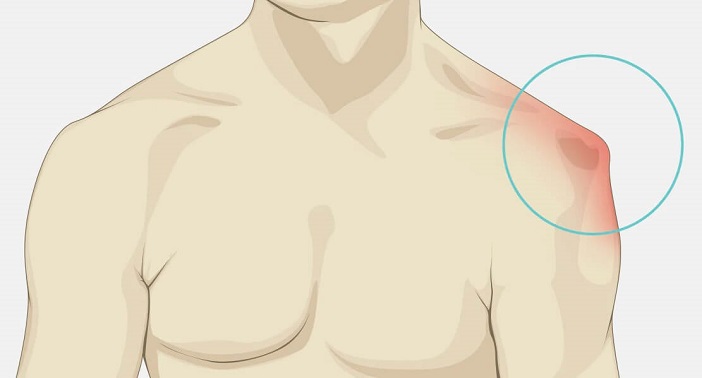
- Severe Pain: One of the most prominent and immediate shoulder dislocation symptoms is severe pain. The pain is typically localized around the shoulder joint and can radiate down the arm
- Visible Deformity: In many cases, a dislocated shoulder can lead to a visible deformity of the shoulder area. The humeral head (the ball-like end of the upper arm bone) may be visibly out of place, causing a noticeable bulge or abnormal contour of the shoulder particularly with an anterior shoulder dislocation. Inferior and posterior shoulder dislocations tend to be less visibly obvious
- Limited Range of Motion: Individuals with a dislocated shoulder often experience a significant reduction in their ability to move the affected arm. This limitation in range of motion is due to the dislocation, as the humeral head is no longer properly positioned within the glenoid socket
- Swelling and Bruising: Swelling and bruising may develop in and around the shoulder joint following a dislocation. This is a result of the injury and the body's inflammatory response. Swelling can contribute to the feeling of tightness and discomfort in the shoulder region
- Numbness or Tingling: Some individuals may experience numbness or tingling in the affected arm as part of their dislocated shoulder symptoms, particularly if there is pressure on nerves or blood vessels near the dislocated joint. This sensation is often temporary but should still be addressed promptly
- Weakness: Due to the pain and instability associated with a dislocated shoulder, individuals may notice weakness in the affected arm. This weakness can make it challenging to perform even basic tasks
- Difficulty or Inability to Move the Arm: In severe cases, individuals may find it virtually impossible to move the dislocated arm. The shoulder joint may feel "locked" in its displaced position, preventing any meaningful movement
- Instability: Some individuals may describe a sensation of shoulder "instability," where the joint feels loose or like it may give way. This feeling can persist even after the shoulder has been reduced (put back into its proper position).
It's important to seek immediate medical attention if you have these dislocated shoulder symptoms as early intervention can lead to better outcomes. Attempting to relocate the shoulder joint yourself is not recommended, as it can lead to further injury or complications.
Dislocated Shoulder Diagnosis

A dislocated shoulder is usually diagnosed by your doctor through a combination of medical history, clinical evaluation and imaging studies.
Your doctor will start by asking you about the circumstances of the injury including when and how it happened and whether you have had any prior shoulder problems, including previous dislocations.
They will also want to know about your current symptoms such as pain, tingling or numbness in the arm and functional limitations.
They will then carry out a physical examination, starting by assessing the appearance of the shoulder, checking for any visible deformities or abnormalities. They will ask you to move your arm in different directions, comparing the range and quality of movement to your other shoulder. They will also look at the sensation, strength and blood circulation in the affected arm to assess for any nerve or blood vessel damage.
You may also be sent for imaging studies such as:
- X-rays: X-rays are commonly used to confirm the diagnosis of a shoulder dislocation and to assess the alignment of the bones. They can reveal the position of the humeral head relative to the glenoid socket and any associated bony damage
- CT Scan: In some cases, a computed tomography (CT) scan may be ordered, especially if there are concerns about associated injuries or if the dislocation is complex
- MRI: Magnetic resonance imaging (MRI) may be used to assess soft tissue damage, such as labral tears, ligament injuries, or rotator cuff injuries, which can occur alongside a dislocation
#CommissionsEarned from Amazon on qualifying purchases
Shoulder Dislocation Treatment
Dislocated shoulder treatment typically involves a combination:
1. Reduction (Repositioning)
The primary goal with treatment for a dislocated shoulder is to put the humeral head back into its normal position within the glenoid socket. This is known as closed reduction.
Shoulder reduction is usually performed by a trained medical professional, such as an emergency room physician or orthopedic specialist.
The process involves gentle manipulation and traction to guide the humeral head back into place. This can be done manually or with the assistance of imaging, like X-rays, to ensure proper alignment.
2. Pain Management
Dislocated shoulders are often associated with severe pain. Pain management is an essential part of treatment and may involve medications, such as over-the-counter pain relievers or prescription painkillers, as prescribed by a healthcare provider. Regularly applying ice packs can also really help reduce pain and swelling.
3. Immobilization

After reduction, the shoulder is typically immobilized in a special sling or brace to keep the shoulder stable, allow for healing and prevent re-dislocation.
You will be able to take the sling off for short periods to do mobilisation exercises to prevent stiffness in the shoulder, elbow and wrist.
The duration of immobilization varies depending on the specific injury and the healthcare provider's recommendations, but may last for a few weeks.
4. Physical Therapy
Physical therapy rehab for shoulder dislocation plays a crucial role in the treatment and recovery. Once the initial pain and swelling have subsided, a physical therapist will guide you through a rehab program:
- Mobility Exercises: to improve range of motion in the arm,
- Strengthening Exercises: to strengthen the muscles around the shoulder
- Stability Exercises: to enhance shoulder stability.
Effective rehab for shoulder dislocation is essential for preventing future dislocations and restoring full shoulder function.
5. Avoiding Re-injury
It's essential to follow your healthcare provider's advice regarding activity restrictions and exercises during the recovery period. Avoid activities that could put excessive strain on the shoulder or increase the risk of re-dislocation e.g. heavy lifting, overhead arm movement and contact sports, especially in the early stages of healing.
Shoulder Dislocation Surgery
Surgery for a dislocated shoulder aims to both repair and stabilize the shoulder joint to reduce the risk of further injury.
Shoulder dislocation surgery is typically carried out when conservative treatments like immobilization and physical therapy have not been effective, with recurrent dislocations or if there is associated damage to the soft tissue or bony structures.
There are various options for shoulder dislocation surgery, depending on the specific condition and individual patient factors including:
- Bankart Repair: This is a common surgical procedure for recurrent anterior shoulder dislocations. It involves repairing a Bankart lesion, where the ring of cartilage that deepens the glenoid socket has torn or become detached, and tightening the shoulder joint capsule. The surgeon reattaches the labrum to the glenoid using sutures or anchors. Bankart repair helps restore stability to the anterior part of the shoulder joint
- Capsulorrhaphy: Capsulorrhaphy, also known as a capsular shift or capsular plication, involves tightening and repositioning the joint capsule to enhance shoulder stability. This procedure is often used in cases of chronic shoulder instability. It reduces the size of the joint capsule, making it tauter and less prone to excessive movement
- Latarjet Procedure: The Latarjet procedure is performed to address recurrent anterior shoulder instability, especially in cases with significant bone loss on the glenoid. During this shoulder dislocation surgery, a piece of bone from the coracoid process (a part of the shoulder blade) is transferred and fixed to the front of the glenoid to create a "bony block" that prevents further dislocations
- HAGL Repair: HAGL stands for "humeral avulsion of the glenohumeral ligament." In this procedure, the surgeon repairs the ligament that attaches to the humerus to the glenoid socket which is often torn during a shoulder dislocation to help restore stability to the shoulder joint
- SLAP Repair: SLAP (Superior Labrum Anterior to Posterior) tears involve damage to the upper part of the labrum where the biceps tendon attaches. Repair of a SLAP tear may be necessary as part of shoulder dislocation surgery in cases of recurrent instability or persistent pain
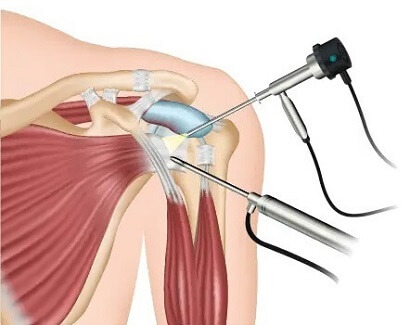
Many of these surgical procedures can be performed arthroscopically (keyhole surgery), using minimally invasive techniques with small incisions and a camera for visualization. However, in some cases, open surgery with a larger incision may be necessary for better access and repair.
The choice of surgical procedure depends on factors such as the type of shoulder instability, the extent of tissue damage, the patient's age and activity level, and the surgeon's expertise.
Dislocated Shoulder Recovery
Dislocated shoulder recovery time can vary significantly depending on the direction and extent of the injury but typically follows this pattern:
- First Few Days: the first step with dislocated shoulder recovery is pain management with medication, ice packs and elevation to reduce swelling, immobilization in a sling/brace, and avoiding any strenuous activities or movements
- Weeks 1-6: as pain decreases you can start physical therapy which will involve gentle exercises to maintain and improve shoulder and arm mobility, strength and stability. You will gradually start to wean off the sling/brace as guided by your healthcare provider
- Weeks 6-12: physical therapy progresses to more advanced strengthening and stability exercises to rebuild muscle strength, flexibility and endurance. You probably won’t need to wear the sling/brace anymore. You may be able to start a gradual return to light activities
- Months 3-6: dislocated shoulder recovery at this stage focuses on functional activities related to your usual daily activities or respective sports, focusing on further strengthening and stability work. The timeline for returning to sports can vary widely depending on individual progress and the nature of the sport
- Months 6-12: high level rehab programmes will focus on getting you back to your pre-injury level of sports to ensure a full recovery. Ongoing maintenance exercises are important to keep the shoulder strong and flexible to reduce the risk of re-injury
Factors Affecting Recovery Time
There are a number of things that can affect dislocated shoulder recovery time:
- Type Of Dislocation: partial dislocations will recover much quicker than full dislocations. Posterior shoulder dislocations typically take longer to recover from than anterior dislocations as they tend to be associated with higher impact injuries which cause more severe associated injuries
- Associated Injuries: such as fractures or soft tissue damage will increase recovery time
- Adherence To Rehab: how well you stick to your physical therapy programme can have big impact on shoulder dislocation recovery time. It can be tempting to cut corners, skip days and stop treatment early but this will slow down your recovery and make you more prone to re-injury
- Individual Factors: like age, overall health, and pre-existing shoulder conditions can affect recovery time
- The Need For Surgical Treatment: if surgery was required, it is generally because there was more extensive damage so the recovery time may be longer
Recovery time can range from a few weeks for a simple, uncomplicated dislocation to several months or longer for more complex injuries or for those aiming to return to high-demand activities. It's crucial to follow the advice and recommendations of healthcare providers and physical therapists throughout the recovery process to optimize outcomes and minimize the risk of recurrent dislocations or long-term complications.
Remember that every person's healing process and dislocated shoulder recovery time will be different and you may experience fluctuations in your road to recovery. Don’t overlook your achievements during the recovery process, no matter how small they may seem. Every little progress is a step towards independence and full dislocated shoulder recovery - celebrating them can maintain your enthusiasm and keep your morale high.
Dislocated Shoulder Summary
A dislocated shoulder is when the ball-shaped head of humerus at the top of the upper arm bone pops out of the shoulder socket. The shoulder is the most mobile joint in the body but also the least stable making the shoulder the most likely joint to dislocate.
Shoulder dislocations are usually caused by high-impact accidents e.g. fall or sporting injury. Muscle weakness or imbalance and joint laxity can increase the risk of shoulder dislocations.
Common dislocated shoulder symptoms include immediate severe pain at the time of injury, obvious deformity at the shoulder with associated bruising and swelling, difficulty or complete inability to move the arm.
Shoulder dislocation treatment typically involves relocating the joint, temporary immobilisation in a sling/brace, pain management, exercises and in some cases surgery.
Physical therapy rehab for shoulder dislocation is a vital part of treatment including progressive strengthening, stability and stretching exercises as you move through the recovery process.
Dislocated shoulder recovery time varies and regaining total function of your shoulder post-dislocation will take time and patience—usually several weeks to months. Recovery will depend largely on the extent of damage to the shoulder and adherence to the treatment plan.
SAFETY ADVICE: You should seek medical help immediately if you suspect you have dislocated your shoulder. Delaying can potentially cause more damage to your shoulder joint and surrounding tissues such as nerves and blood vessels.
You may also be interested in the following articles:
Related Articles
Page Last Updated: May 16th, 2024
Next Review Due: May 16th, 2026