- Home
- Wrist Pain Diagnosis
- Boutonniere Deformity
Boutonniere Deformity
Written By: Chloe Wilson BSc (Hons) Physiotherapy
Reviewed By: SPE Medical Review Board
Boutonniere deformity, aka buttonhole finger, is a common finger deformity that affects the position of the middle joint.
It usually develops after a tendon injury or as a result of inflammatory arthritis and can gradually worsen if left untreated.
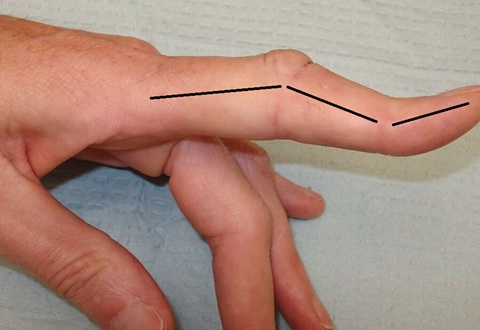
With classic boutonniere deformities, the middle joint of the finger gets stuck in a bent position while the fingertip bends backwards.
In this article, I’ll explain what boutonniere deformity is, what causes it, the typical symptoms, how it’s diagnosed, and the best treatment options, including splinting and surgery.
What Is Boutonniere Deformity?
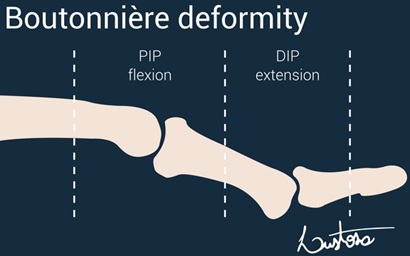
Boutonniere deformity occurs when the middle joint of the finger (PIP joint) becomes stuck in a bent position, while the end joint (DIP joint) bends backwards into hyperextension.
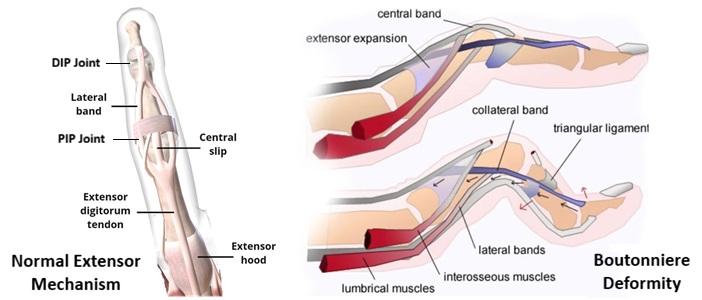
This happens when the central slip of the extensor tendon is damaged or stops functioning properly. The central slip/band normally runs over the top of your finger, with lateral bands that run down the side, and allows you to straighten the middle joint of your finger.
Overstretching or tearing the central slip splits the tendon. The proximal phalanx "buttonholes" between the lateral bands of the extensor tendon, like a button passing through a buttonhole. This stretches the triangular ligament.
As a result:
- The PIP joint flexes and cannot be actively straightened
- The DIP joint is pulled into hyperextension
- Normal finger balance and function are lost
This imbalance creates the classic boutonniere deformity where the middle finger joint is bent and the fingertip bends backwards.
Boutonniere deformity most commonly affects the fingers, but a similar problem can occasionally affect the thumb, sometimes referred to as a boutonniere thumb deformity.
If the central slip injury is not treated early, the deformity can become fixed and permanent.
Causes Of Boutonniere Deformity
Boutonniere deformity is usually caused by a traumatic injury that disrupts the central slip of the extensor tendon on the back of the finger. Common causes include:
Finger Injuries
- Jammed or “stoved” fingers - direct blow to the fingertip strains the tendon
- Finger fracture or dislocation that stretches or tears the tendon
- Lacerations on the finger that cut through the central slip
- Sports injuries, particularly ball sports
Other Causes
- Rheumatoid arthritis: chronic inflammation weakens the extensor tendon over time. Often affects multiple fingers
- Untreated or poorly managed tendon injuries
- Long-standing finger imbalance
- Burns or infections that lead to weakening and/or scarring of the tendon
In some cases, the initial injury may seem minor, with the deformity only becoming obvious weeks later.
Boutonniere Deformities Symptoms
Symptoms of boutonniere deformity may appear immediately after injury or develop gradually over time, particularly in people with arthritis.
Common symptoms include:
- A bent middle finger joint (PIP joint) that won’t fully straighten
- Hyperextension of the fingertip joint (DIP joint)
- Pain and tenderness over the middle joint
- Swelling around the PIP joint
- Stiffness, especially in the morning
- Reduced grip strength
- Difficulty performing fine motor tasks
- Inability to actively straighten the finger
Early on, the finger may still be flexible and can be straightened with assistance. Over time, the deformity may become stiff and fixed.
Boutonniere Deformity Diagnosis
Buttonhole finger is usually diagnosed through a clinical examination by a doctor, hand therapist, or orthopaedic specialist.
Clinical Assessment
Diagnosing boutonniere deformities typically involves:
- Observing finger posture at rest
- Assessing active and passive movement of the finger joints
- Testing extensor tendon function
- Checking whether the PIP joint can be straightened
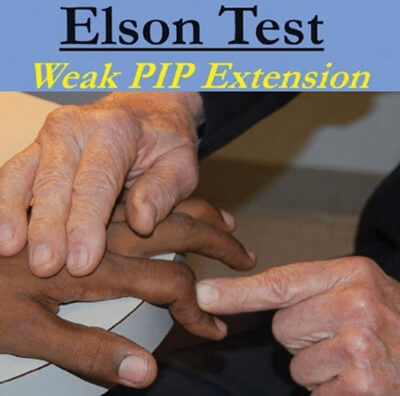
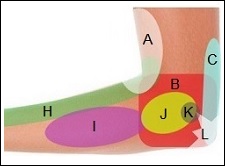
Elson Test
The Elson test can be used for early detection of central slip injuries, and can diagnose this injury before the deformity sets in.
- The patient rests their hand on the edge of a table, with the PIP joint bent to 90 over the edge
- The patient is asked to extend their finger against resistance
Central Slip Intact: Finger extends with no obvious weakness
and fingertip remains floppy
Central Slip Damaged: finger extension is weak and fingertip
pulls up into hyperextension and is stiff
A classic sign is the inability to actively extend the PIP joint, even when passive movement is still possible in early cases.
Imaging Studies
Imaging is not always necessary but may be used to:
- Rule out fractures after trauma
- Assess joint damage in arthritis
- Identify associated tendon or avulsion injuries
This may include X-rays, or occasionally ultrasound or MRI in more complex cases.
When To See The Doctor
You should seek medical advice if you notice any signs of boutonniere deformities, particularly following a finger injury.
See a doctor or hand specialist if:
- Your middle finger joint stays bent
- You can’t straighten the finger on your own
- The finger was jammed, struck, or cut over the middle joint
- Pain or swelling persists beyond a few days
- The finger shape is gradually worsening
- You have rheumatoid arthritis and notice finger deformity
Boutonniere Deformity Treatment
Early treatment is important, as buttonhole finger responds best when addressed promptly, before stiffness creeps in.
If the deformity is left untreated for more than 3 weeks, treatment becomes much more complicated and full recovery is less likely.
1. Non-Surgical Treatment
Early-stage boutonniere deformity is usually treated successfully without surgery. This may include:
- Continuous Splinting: to keep the tendons in the right position. Usually 6-8 weeks
- Hand Therapy or Physical Therapy: to regain full strength and motion
- Managing Inflammation In Arthritis: e.g. medications or corticosteroid injections
The aim is to restore tendon balance and prevent joint stiffness.
2. Boutonniere Deformity Splint
A boutonniere deformity splint is the mainstay of early treatment, as it:
- Holds the PIP joint fully straight
- Allows the DIP joint to move freely
- Encourages proper healing of the extensor tendon
Key splinting principles:
- Worn full-time for 6–8 weeks
- Must stay on 24 hours a day
- Even brief bending can disrupt healing
- Often followed by night splinting
Splints may be custom-made or prefabricated and are most effective when started early.
3. Boutonniere Deformity Surgery
Boutonniere deformity surgery is usually reserved for:
- Long-standing deformities with fixed joint contractures
- Failed splinting
- Severe functional impairment
- Tendon is severed (cut)
- Associated bone fragment displacement
Surgical options include:
- Tendon Repair or Reconstruction: if the tendon is cut or torn, it is repaired with sutures
- Avulsion Repair: if a piece of bone is pulled away with the tendon, it is reattached with anchors, sutures or bone tunnels
- Joint Stabilisation: if the joint is dislocated or unstable, temporary pins (K-wires) are placed to hold the joint straight while it heals
- Joint Fusion: in advanced arthritis
Post-operative splinting and hand therapy are essential after surgery to regain full function. Care must be taken as the tendon is vulnerable to re-injury for around 3 months.
Full recovery can take several months, depending on the severity of the injury and rehabilitation.
Long-Term Recovery & Outcome
Boutonniere deformity recovery varies depending on the treatment, time to treatment and underlying cause of the central slip injury.
- Early-treated cases often recover well with minimal long-term issues
- Delayed treatment increases the risk of stiffness and permanent deformity
- People with rheumatoid arthritis may have ongoing joint changes despite treatment
Overall, the outcome for boutonniere deformities is best when it is recognised early and treated promptly, ideally before the joint becomes stiff or fixed.
Boutonniere Deformity vs Swan Neck Deformity
Boutonniere deformity and swan neck deformity are often confused. They are both finger deformities affecting the PIP joint, but they actually affect the finger joints in opposite ways.
| Feature | Boutonniere Deformity | Swan Neck Deformity |
|---|---|---|
| Typical appearance | Middle joint bent, fingertip bends backwards | Middle joint bent backwards, fingertip droops |
| PIP joint | Flexed (bent forward) | Hyperextended (bent backwards) |
| DIP joint | Hyperextended | Flexed |
| Main cause | Central slip injury from finger trauma or arthritis | Tendon/ligament imbalance, laxity, or arthritis |
| Early treatment | PIP extension splint | Prevent PIP hyperextension |
Although the deformities look different, both conditions can affect hand function and grip. Correct diagnosis is important, as treatment and splinting strategies differ for boutonniere and swan neck deformities.
Boutonniere Deformity Summary
Boutonniere deformity, aka buttonhole finger, is a condition caused by injury to the central slip of the extensor tendon. It leads to a bent middle finger joint (PIP joint) and hyperextension of the fingertip (DIP joint).
It commonly develops after finger injuries or in people with inflammatory arthritis. When diagnosed early with the Elson test, boutonniere deformity treatment, particularly continuous splinting of the PIP joint, is often highly effective and can prevent permanent deformity.
Delayed or untreated cases may become fixed and require boutonniere deformity surgery, followed by hand therapy. Early assessment is key, as prompt treatment offers the best chance of restoring normal finger alignment and function.
You may also be interested in the following articles:
Related Articles
Shoulder Diagnosis
June 25th, 2025

Wrist Diagnosis
December 4th, 2025
Elbow Diagnosis
February 28, 2025
Medical & Scientific References
- Boutonniere Injury. British Society For Surgery Of The Hand
- Boutonniere Deformity. Royal United Hospitals Bath NHS Foundation Trust
- Boutonniere Deformity. National Library For Medicine - NIH.
Page Last Updated: January 28th, 2026
Next Review Due: January 28th, 2028