- Home
- Wrist Pain Diagnosis
- Swan Neck
Swan Neck Deformity
Written By: Chloe Wilson BSc (Hons) Physiotherapy
Reviewed By: SPE Medical Review Board

A swan neck deformity is a common condition where the fingers bend abnormally.
It often develops gradually and can affect hand function, grip strength, and everyday activities. It may affect one or more fingers.
Swan neck finger is most often linked with arthritis, tendon imbalance, or untreated finger injuries, but it can also occur after trauma or neurological conditions.
Understanding what causes swan neck deformity, common symptoms, how it differs from similar finger problems and the best treatment options is key to making a good recovery.
What Is Swan Neck Deformity?
Swan neck deformity is a degenerative finger condition where:
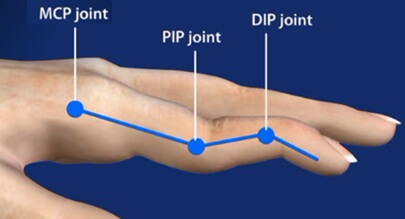
- The middle joint (PIP joint) bends backwards into hyperextension
- The fingertip joint (DIP joint) bends downwards into flexion
- The knuckle joint (MCP joint) may also bend downwards
This creates the classic “swan neck” appearance, similar to the curve of a swan’s neck, hence the name. It is the opposite of a boutonniere deformity.
Swan neck disease affects the balance of tendons and ligaments that control finger movement. When this balance is lost, the finger can no longer straighten and bend normally. Over time, the deformity may become fixed and difficult to correct.
Although most common in the fingers, swan neck thumb deformity can also occur, particularly in people with rheumatoid arthritis.
Nalebuff Classification
Swan neck deformity is commonly described using the Nalebuff classification, which categorises the condition based on PIP joint flexibility in different MCP joint positions, helping guide treatment decisions.
- Type I: flexible, correctable deformity in all positions
- Type II: persistent PIP hyperextension with limited bending in certain positions
- Type III: fixed, stiff deformity in all positions
- Type IV: severe joint damage affecting both PIP and DIP joints.
What Causes Swan Neck Deformity?
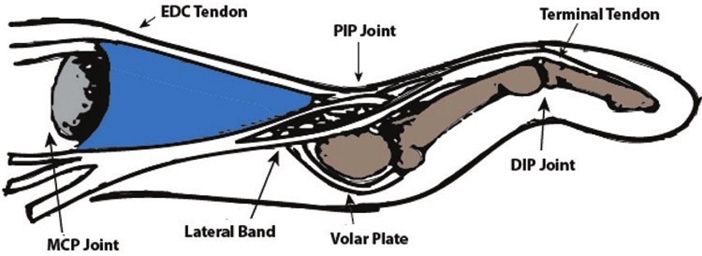
Finger joint deformities occur when the delicate system that controls finger movement is damaged.
This system, known as the extensor mechanism, is a network of tendons and muscles that work together to move and control the finger joints.
Because these structures are carefully balanced, a problem in one part affects the others. If one joint loses the force that normally controls it, another joint may be pulled too strongly in the opposite direction.
Swan neck deformity develops when:
- The extensor tendon on the back of the finger is damaged or weakened
- The volar plate ligament on the palm side of the finger is stretched or torn and becomes lax
- There is resultant tightness in the triangular ligament around the PIP
- Finger muscles become overly tight and shortened (contracture)
Common causes of swan neck deformity fingers include:
- Arthritis: joint inflammation damages the soft tissues, weakening the tendons, leading to progressive deformity. Rheumatoid arthritis is the most common cause of swan neck deformity finger, and up to 50% of people with RA will develop it
- Finger Injuries: such as untreated mallet finger, chronic joint sprains, laceration or previous finger fractures
- Neurological or Muscle Conditions: such as stroke, cerebral palsy, Parkinson’s, muscle spasticity
Swan neck deformity may affect one finger, multiple fingers, or the thumb, depending on the underlying cause.
Symptoms of Swan Neck Deformity
Swan neck finger symptoms usually develop gradually and may worsen over time:
- Middle joint of the finger bends backwards, forming a valley
- Fingertip bends forwards, forming a peak
- Progressive finger stiffness or locking
- Difficulty making a fist and with fine motor tasks like buttoning or writing
- Weak grip and reduced pinch strength
- Pain or swelling (especially with arthritis)
- Snapping feeling when moving the finger
In advanced cases, the finger may become fixed in the deformity, making movement very limited.
Diagnosis
Swan neck disease diagnosis is based on a clinical history and physical examination. Your clinician will ask about symptom onset, progression, previous finger injuries, and signs of arthritis.
They will then carry out a clinical examination where they will:
- Assess finger posture and active/passive movement
- Test joint stability
- Look for signs of arthritis or tendon imbalance
You may also be sent for imaging studies or tests to confirm the diagnosis or rule out other conditions:
- X-rays may be used to assess joint damage or arthritis
- Ultrasound or MRI may be used if tendon injury is suspected
- Blood Tests to help diagnose inflammatory diseases
Early diagnosis is important, as treatment is far more effective before the deformity becomes rigid.
Swan Neck vs Boutonniere Deformity vs Mallet Finger
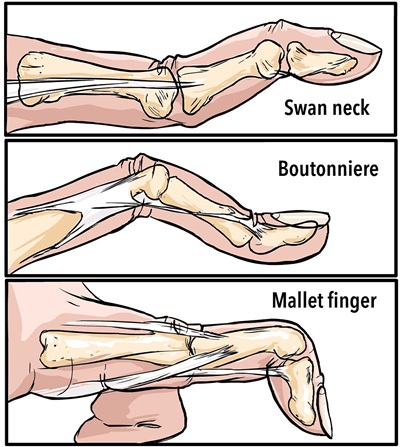
Although these conditions affect similar joints in the fingers, they are caused by different tendon problems and require different treatment.
- Swan Neck Deformity: Middle joint bends backwards, fingertip droops
- Boutonniere Deformity: Middle joint bends forward, fingertip bends backwards
- Mallet Finger: Fingertip droops due to extensor tendon injury
Correct diagnosis is essential, as splinting the wrong joint can make symptoms worse.
| Feature | Swan Neck Deformity | Boutonniere Deformity | Mallet Finger |
|---|---|---|---|
| Affected Joints | PIPJ hyperextension, DIPJ flexion, MCPJ flexion | PIPJ flexion, DIPJ hyperextension | DIP joint flexion only |
| Primary Tendon Problem | Imbalance of extensor and flexor tendons; often lateral band migration | Central slip of the extensor tendon rupture | Extensor tendon rupture at the fingertip |
| Common Causes | Rheumatoid arthritis, mallet finger, trauma, neurological disorders | Trauma, rheumatoid arthritis, lacerations | Sudden force to fingertip, sports injury, laceration |
| Flexibility | May be flexible in early stages; can become fixed | Initially flexible, may become fixed if untreated | Fixed droop of DIP until treated |
#CommissionsEarned from Amazon on qualifying purchases
Swan Neck Deformity Treatment
Swan neck finger treatment depends on the underlying cause, how flexible the finger is and how long the deformity has been present.
Non-Surgical Treatment
For flexible or early-stage deformities:
- Splinting to support the middle joint
- Hand therapy exercises to improve tendon balance e.g. tendon gliding exercises
- Anti-inflammatory treatment for arthritis
- Activity modification to reduce strain
Early swan neck treatment can often slow progression and improve function, even if the deformity cannot be fully reversed.
Splint for Swan Neck Deformity
A swan neck deformity splint is commonly used as part of treatment.
Swan neck splints work to correct the finger position by:
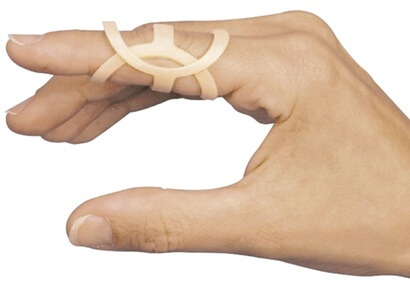
- Preventing hyperextension of the middle joint
- Allowing controlled finger flexion
- Improving grip and hand function
Common options include:
- Double Ring splints
- Custom thermoplastic splints
Splints are particularly helpful for people with rheumatoid arthritis or early deformity, and may delay or avoid the need for surgery.
Swan Neck Surgery
Swan neck surgery is usually considered when the deformity is severe, fixed, or painful, and non-surgical treatment hasn’t helped.
Surgical options include:
- Tendon Reconstruction: Repairs or repositions tendons to correct alignment.
- Volar Plate/Ligament Tightening: Prevents the middle joint from bending backward.
- Joint Fusion: Stabilises severely arthritic joints but removes movement.
- Joint Replacement: Replaces damaged joints with an implant to reduce pain and maintain some motion.
The goal of swan neck finger surgery is to restore balance, reduce pain, and improve hand function, rather than achieving a perfectly straight finger.
What to Expect After Surgery
- Recovery: Recovery can take several weeks to months. Finger stiffness and swelling are common initially.
- Rehabilitation: Hand therapy is essential after surgery to regain motion, strength, and fine motor skills.
- Splinting: Temporary splints or buddy taping may be used to protect the repair during healing.
- Results: Most patients achieve improved hand function, better alignment, and reduced pain, although some residual stiffness may remain.
Surgery is most successful when the procedure is tailored to the specific cause of the deformity and combined with post-operative rehabilitation. Early consultation with a hand specialist is important to determine the best approach.
FAQ’s on Swan Neck Finger
Here are answers to some of the most commonly asked questions about swan neck deformity fingers.
1.
Can swan neck deformity ever go away on its own without treatment?
1. Can swan neck deformity ever go away on its own without treatment?
In most cases, it won’t fully resolve by itself, especially once the joint becomes fixed. Early-stage deformities may improve slightly with splinting and therapy, but spontaneous correction is rare without intervention.
2.
Does swan neck deformity get worse over time if left untreated?
2. Does swan neck deformity get worse over time if left untreated?
Yes - the imbalance in tendons and ligaments can progressively worsen, leading to increased stiffness, reduced movement, and loss of function.
3.
Is swan neck deformity painful?
3. Is swan neck deformity painful?
Pain isn’t always present at first. Many people notice abnormal joint shapes or difficulty using the finger before pain develops. If arthritis or tendon irritation is present, pain, swelling, or snapping sensations may occur.
4. Are certain people more at risk of developing swan neck deformity?
4. Are certain people more at risk of developing swan neck deformity?
People with rheumatoid arthritis are at higher risk, particularly women with RA. Tendon injuries, neurological conditions, or connective tissue disorders can also increase risk.
5. Can swan neck deformity be prevented?
5. Can swan neck deformity be prevented?
While not always preventable, you can reduce risk by managing underlying conditions like rheumatoid arthritis, protecting fingers after injuries, and using early splinting or therapy to maintain joint balance.
6.
How long does recovery take after surgery for swan neck deformity?
6. How long does recovery take after surgery for swan neck deformity?
Recovery depends on the procedure but typically involves weeks to months of splinting and hand therapy before strength and motion are restored.
7.
Can swan neck deformity come back after treatment?
7. Can swan neck deformity come back after treatment?
Recurrence is possible, especially if the underlying cause, such as inflammatory arthritis, isn’t controlled. Long-term therapy and condition management help prevent progression or recurrence.
8.
Does swan neck deformity cause long-term disability or affect quality of life?
8. Does swan neck deformity cause long-term disability or affect quality of life?
With appropriate treatment - splints, therapy, and surgery if needed - many people maintain useful hand function. Some stiffness or limited movement may persist in more advanced cases, but most can perform daily tasks.
Swan Neck Disease Summary
Swan neck deformity is a finger condition caused by tendon and ligament imbalance, most commonly linked to arthritis or untreated finger injuries.
It leads to backward bending of the middle joint and drooping of the fingertip, affecting grip, strength, and hand function.
Early diagnosis and treatment - including splinting, hand therapy, and arthritis management - can significantly improve outcomes. In more advanced cases, surgery may be needed to restore balance and reduce pain.
Swan neck deformity shouldn't be confused with other similar finger conditions such as boutonniere deformity or mallet finger where the finger bends in different directions.
If you notice progressive finger deformity, stiffness, or loss of function, early assessment is key to preventing long-term problems.
You may also be interested in the following articles:
Related Articles
Shoulder Diagnosis
June 25th, 2025

Wrist Diagnosis
December 4th, 2025
Elbow Diagnosis
February 28, 2025
Page Last Updated: January 29th, 2026
Next Review Due: January 29th, 2028